Top 12 FAQ’s: Understanding Living Kidney Donation
1. Who can be a living kidney donor?
Most people in good health can be considered for testing to see if they’d qualify to become a living kidney donor. The qualification process typically begins with a telephone screening that determines if a thorough evaluation should follow. The evaluation typically includes several interviews, exams, scans and lab tests. The transplant center requires these tests to ensure the person who wishes to donate is healthy enough to do so.
2. What’s the kidney donation surgery like? What Are the risks?
The Surgery:
The surgery is performed with small incision, which is known as laparoscopic surgery. In kidney donation (also known as a nephrectomy), the procedure typically involves four 1-inch slits in the area of the stomach and bladder. There is also one four-inch incision made around the navel. This incision is a bit larger, so the kidney can be removed from this area.
Risks:
The surgical process for removing a kidney from a healthy individual has become a fairly standard procedure. Nonetheless, the procedure still carries the same level of risk as any other major surgery. The most common risks associated with kidney donation (also known as a nephrectomy) can include blood clotting, infection and a reaction to the anesthesia. The risk of death from donating a kidney is less than one percent, or 0.0003 % (which is about 3 in every 10,000 surgeries).
Hospital Stay:
Hospital recovery for donating a kidney usually involves 1-3 overnight stays. Hospital discharge is determined by the donor’s health and their ability to get out of bed and walk on their own.
Discomfort:
Because the kidney donor will feel pain after surgery, pain medications will be provided to help patient comfort. It is not uncommon for some patients to experience constipation from pain medication. Because of this, laxatives may be provided.
Work & Activities:
Most living kidney donors can resume their regular activities within 3 weeks after donation, providing they are less strenuous activities. Depending on the type of work the kidney donor performs and the level of difficulty, kidney donors can often go back to work within 3-5 weeks. If the donor’s job is a desk job, they can often get back to work even sooner. Those engaged in more strenuous activities are advised to refrain from difficult physical tasks until they are completely recovered.
3. Who pays for the cost for the kidney donor’s surgery?
The medical insurance covering the individual who receives the donor’s kidney will cover the donor’s medical costs. Things that are not covered or paid for (by the transplant patient’s insurance company) can include the donor’s time off from work, recovery care and travel costs. There are a few states that now require employers to cover living kidney donor’s time off work for a set period of time. *It is wise to check with employer policies, state laws and federal updates.
4. Can a living kidney donor live a normal life after donating?
There are many studies showing living kidney donors doing quite well after they donate a kidney. For the most part, their health and quality of life remains unchanged. The most notable change expressed by most living kidney donors comes in the form of the perpetual joy they feel for their extraordinary act of human kindness.
Living kidney donors aren’t typically required to take new medications following the surgery, other than a pain medication or a stool softener for a short period of time. Likewise, kidney donors do not need to follow a special diet after they are discharged from the hospital. They are, however, asked to avoid alcohol while taking pain medication. The guideline for alcohol consumption after kidney donation is fairly standard. Living kidney donors should be responsible and consume alcohol in moderation.
5. What emotions might the kidney donor feel?
Like any new experience, donors can often feel both excitement and anxiety from time to time. Typically, the more the donor understands going into the process, the less anxiety they’ll experience. Post-surgery, donors often report a feeling of honor and joy. As a result, their uplifting attitudes have been found to reduce post-surgical pain, while also boosting perceptions of recovery inconveniences.
6. How successful are living kidney donor transplants?
Hospitals with established transplant programs show very good transplant success rates. Most transplant centers* exceed a 95% success rate one year after transplantation.
The best success rates are seen in transplants from living kidney donors. (*Transplant programs are required to keep track of their success rates. Be sure to ask the center to share their success rates).
7. How old do you have to be to donate a kidney?
Generally, the ideal age range to donate a kidney is 18-65 years old. Of course, the kidney donor will need to be healthy enough to donate a kidney safely. While there have been donors who have donated a kidney after the age of 65; younger donors are preferred. Family members are also preferred, as they offer a better match.
8. What happens if I’m not a blood-type match?
Often times, potential donors can be incompatible in blood type or have antibodies that would fight against their intended recipient. When the living kidney donor is not an ideal match for their intended recipient they can still donate—just not directly. This is accomplished through a Paired Exchange Program.
In Paired Exchange, a computer algorithm is used to find a better match for incompatible groupings. In this model, the living kidney donor’s kidney is swapped with another person’s incompatible living kidney donor.
There is also something known as Compatible Pairs, where a donor and patient that are biologically compatible (but want to find a better match through a paired exchange swap) agree to be matched with more suitable donors to increase the chance that the transplanted kidney will function better and last longer.
Advanced Donation, also known as ADP, offers a unique kidney paired exchange opportunity, separated in time.
There are four types of ADP cases. 1) Short term cases, where the intended recipient is on dialysis or is in imminent need of a kidney transplant. 2) Short Term Swap Saver, where the paired donor proceeds with donation to keep the rest of a swap on schedule, but the recipient remains in imminent need of a kidney transplant. 3) Voucher cases, where the intended recipient is currently not in need of a kidney transplant, yet they may need a transplant in the future; and the 4) Voucher Swap Saver, where the donor proceeds with donation to keep the rest of a swap on schedule. This occurs after their intended recipient is transplanted by kidney from another living donor or a deceased donor.
9. What if a kidney donor changes their mind?
Potential donors are able to change their mind about moving forward before or after they’ve been approved. When this is the case, the reasons for donor disqualification are kept confidential. The donor’s intended recipient will only be told that the donor was not an ideal candidate, (just as they would if the donor was not medically suitable for donation). To ensure donor privacy, the transplant center does not share the reason as to why a donor was disqualified.
10. How will donating a kidney impact future pregnancies or my sex life?
Donating a kidney has not been shown to reduce the fertility of men or women. Because the body requires time to recover from the surgery of donating a kidney, it is recommended that women wait 3-6 months after donation to get pregnant. However, a donor can engage in sexual activities after their incisions have completely healed and they feel comfortable enough to do so.
11. Are kidney donors rewarded for their gift-of-life?
Legally, there can be no payment given for a kidney donation. There is, however, a high value of perpetual joy that comes with saving someone’s life. Most donor’s say they never expected a financial reward. They have also said that the pride and joy they receive is priceless. Some donors have even called their kidney donation their own “Mount Everest.” Living kidney donation is a very personal experience. Because of this, not everyone can qualify to be a living kidney donor. While potential donors don’t have to be a the bravest and most heroic people on earth to consider living kidney donation, they’re dubbed as heroic, world-class humanitarians for life, post-donation.
12. What’s the first step to see if I’d qualify to be a living kidney donor?
If you know someone in need of a kidney transplant, the first step would be to call the kidney patient’s designated transplant center to schedule a telephone screening. If you don’t know someone in need, and want to donate altruistically, simply contact a transplant center near you.
During the call individuals can ask questions and get more details about the tests involved, the surgical procedure and recovery. Even if the person calling is not completely sure they want to proceed, this call can provide insight to help them decide if living kidney donation is right for them.
All donor coordinator conversations are handled in strict confidence to ensure callers can ask questions without pressure or concern. In other words, their intended recipient will never know someone called in (or their testing status), unless the potential donor communicates directly to their intended recipient.
Back-Up Donors are Important Too!
If someone has been told they are not needed (at this time), but they’re still interested in donating, they can offer to be a “back-up.” This is important, should the intended donor unexpectedly change their mind or become disqualified. (Often times, it takes several potential donors to be tested before a qualified match is found).
Even after the surgery, when back-up donors are no longer needed, they can consider helping someone else. They can do this as an altruistic donor, or participate in a Paired Exchange to help several people by becoming the missing link in the chain.
Benefits of Receiving a Transplant from a Living Donor:
1. Kidney Donors End the Wait:
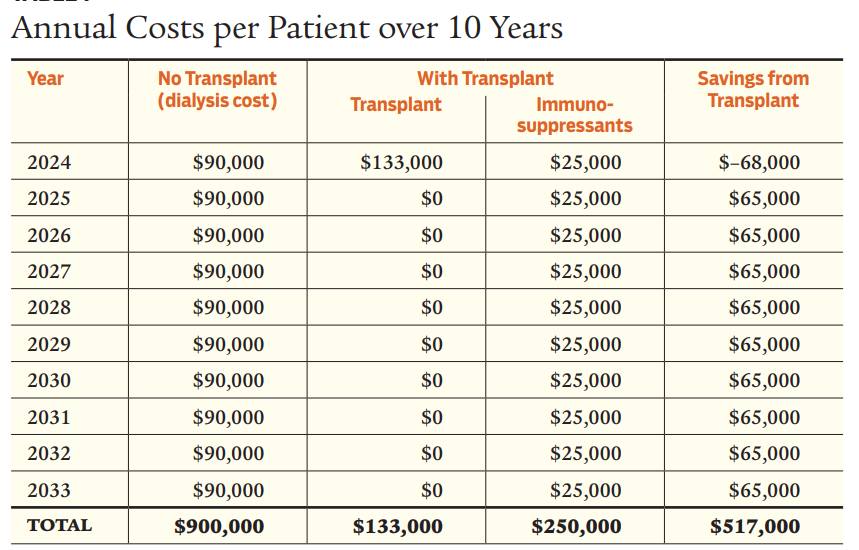
A kidney from a living donor “Ends the Wait” for those in need of a kidney transplant. The surgery can also be scheduled when the kidney patient needs it most—and before the recipient’s health declines to a point of permanently losing their transplant eligibility.
2. Kidney Donors Offer A Better Match:
Living kidney donors are thoroughly tested to ensure the best match for their recipients. Donor testing also minimizes potential risks for both the living kidney donor and their transplant recipient.
3. Kidneys From Living Donors Function Better:
Kidneys from living donors are known to function immediately after transplant. They can also last twice as long as kidneys from deceased donors. This could potentially equate into an additional 10-12 additional years of function.
4. Living Kidney Donors Give Their Recipient an Opportunity to Bypass Dialysis (or eliminate their need):
Since the wait for a kidney from a deceased donor can take from 3 to 9 years or more, they must be on dialysis while waiting just to stay alive. Because of this, living kidney donors can help them end their wait for a transplant and need for continued dialysis. Ideally, when the timing is right, living kidney donors allow their intended recipients to schedule their transplant before they’d require dialysis (known as a preemptive transplant).
Are You a Kidney Patient Hoping to Find a Donor?
Need a living kidney donor for your transplant but don’t know where to start? Have you been told to ask your family and friends, but just thinking about that unimaginable “ask” causes you to shudder? If so, listen up!
What if you could find a way to attract potential donors without ever having to ask anyone to give up a kidney?
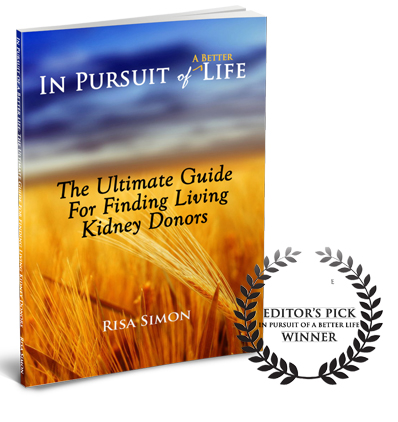
Well, now you can—and this book shows you how! Whether you’re trying to avoid dialysis or end your wait for a transplant, In Pursuit of a Better Life: The Ultimate Guide for Finding Living Kidney Donors is the book you need.
Inside this book for those seeking a living kidney-donor transplant, you’ll discover:
•Conversation starters
•Key talking points
•Story-scripting strategies
•Message outreach tactics
•Enlisting networking teams for story-share
•Phrasing inspirational letters, signs & cards
•Positive mindsets for promoting human kindness
Fellow kidney patient, and author Risa Simon, understands your journey more than most. As a successful preemptive transplant recipient, she shares actionable tips and meaningful insights on how to become your own best advocate and attract your best life possible. The life Risa now lives.
In Pursuit of a Better Life has been called the quintessential marketing plan for engaging in “life conversations” with care, knowledge, and compassion. This book has been described as a lifesaving “game-changer” by those who uncover its proven path to preemptive (before dialysis) live-donor kidney transplants. So, what are you waiting for? If you want to ignite your Donor-Magnet® superpowers by putting these rarely discussed before insights into action—take your hand off the “pause” button and start reading this book! Get yourself a eBook copy today!
Order eBook Below:
If you prefer a Paperback book, link here:





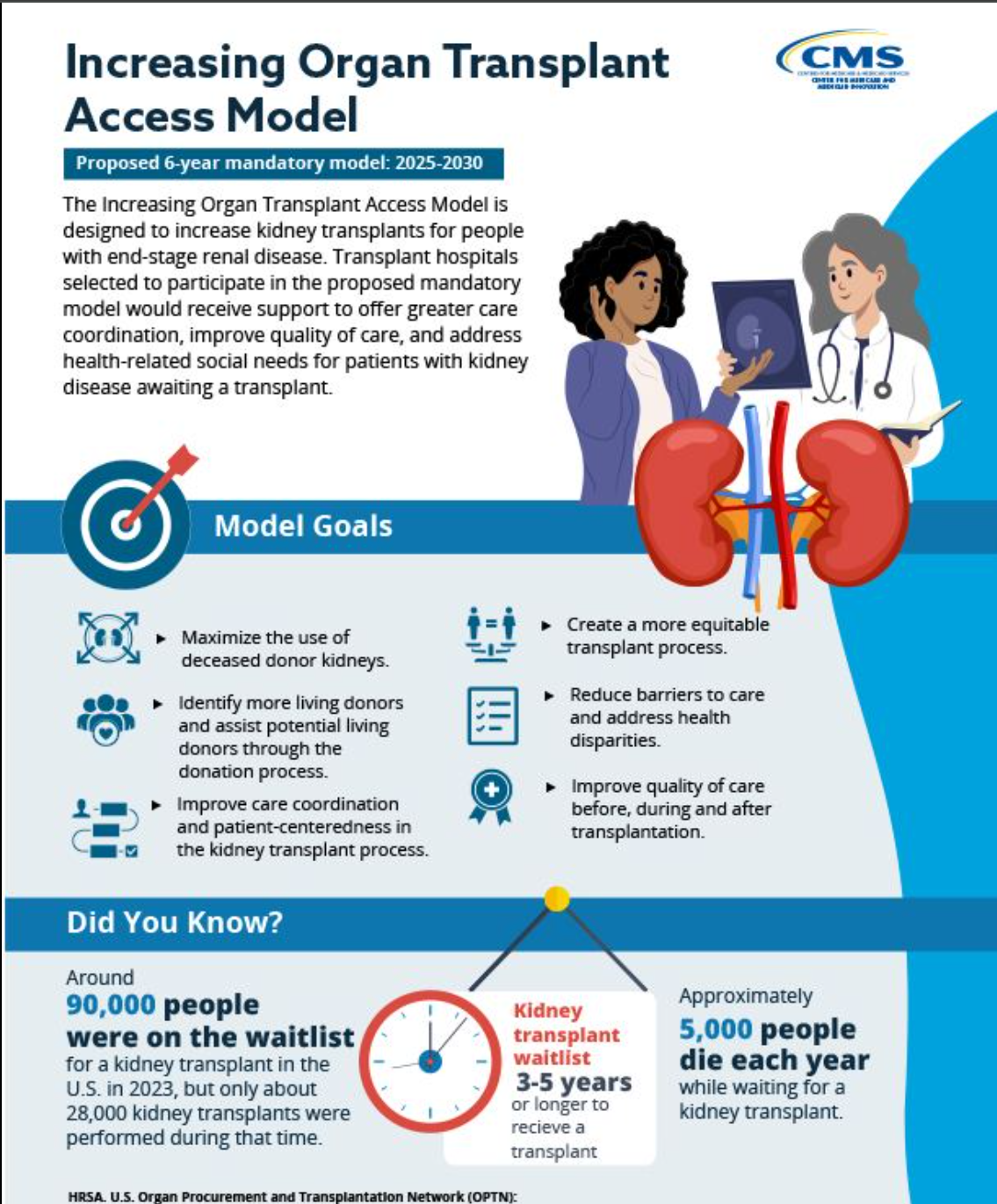
 Increasing Organ Transplant Access (IOTS) Model. Medicare 2025-2030. Key Takeaways:
Increasing Organ Transplant Access (IOTS) Model. Medicare 2025-2030. Key Takeaways:

 These days, securing a kidney transplant—before dialysis, requires more luck than medical qualifications. It seems that the biggest barrier to transplant is not so much disqualifying health factors, as much as it is about knowing how to proactively secure a transplant before dialysis is required.
These days, securing a kidney transplant—before dialysis, requires more luck than medical qualifications. It seems that the biggest barrier to transplant is not so much disqualifying health factors, as much as it is about knowing how to proactively secure a transplant before dialysis is required.

 TransplantFirst Academy (TFA) takes great pride in bringing an initiative for Living Donor Protections to Arizona’s lawmaker’s ears. Thanks to passionate sponsors, Senators Carter and Brophy McGee, and Arizona’s lawmakers who voted in support of the bill for living organ donor protections, Gov. Ducey signed SB1100 into law last week.
TransplantFirst Academy (TFA) takes great pride in bringing an initiative for Living Donor Protections to Arizona’s lawmaker’s ears. Thanks to passionate sponsors, Senators Carter and Brophy McGee, and Arizona’s lawmakers who voted in support of the bill for living organ donor protections, Gov. Ducey signed SB1100 into law last week.