Donor Magnet Pro’s are hopeful recipients and outreach teams who know how to enlighten listeners about what it takes to become a living kidney donor. This Top 12 FAQ List was recreated to help you share insights on what’s involved in living kidney donation.
- Who can be a living kidney donor?
Most people in good health can be evaluated to be considered as a living kidney donor. The qualification process typically begins with an online or telephone screening that determines if a thorough evaluation should follow. The evaluation typically includes several interviews, exams, scans and lab tests. The transplant center requires these tests to ensure the person who wishes to donate is healthy enough to do so.
- What does the process involve?
The Surgery:
The surgery is performed with small incisions, which is known as a laparoscopic surgery. In kidney donation (also known as a nephrectomy), the procedure typically involves four 1-inch slits in the area of the stomach and bladder. There is also one four-inch incision made around the navel. This incision is a bit larger, so the kidney can be removed from this area.
Risks:
The surgical process for removing a kidney from a healthy individual has become a fairly standard procedure. Nonetheless, the procedure still carries the same level of risk as any other major surgery. The most common risks associated with kidney donation (also known as a nephrectomy) includes blood clotting, infection and a reaction to the anesthesia. The risk of death from donating a kidney is less than one percent, or 0.0003 % (which is about 3 in every 10,000 surgeries).
Hospital Stay:
Hospital recovery usually involves 1-3 overnight stays. Discharge is determined by the donor’s health and their ability to get out of bed and walk on their own.
Discomfort:
Although the donor will feel pain after surgery, pain medications will be provided to help patient comfort. It is not uncommon for some patients to experience constipation from pain medication. When this is the case, laxatives are provided. FAQ: Understanding Living Kidney Donation.
Most living kidney donors can resume their regular activities within 3 weeks after donation. Depending on the type of work they perform, they can often go back to work within 3-5 weeks. If the donor’s work is office work, they can often get back to work even sooner. Those engaged in more strenuous activities are advised to refrain from these types of tasks until they are completely recovered.
- Who is going to pay for the cost of the procedure?
The medical insurance covering the individual who receives the donor’s kidney (and kidney transplant procedure) will also cover the donor’s medical costs. Things that are not covered or paid for (by the transplant patient’s insurance company) is the donor’s time off from work and travel costs. There are a few states that now require employers to cover living kidney donor’s time off work for a set period of time. *It is wise to check with employer policies, state laws and federal updates to ensure both donor and recipient are up-to-date.
- Can a donor still live a normal life after surgery?
There are many studies showing living kidney donors doing quite well after they donate a kidney. For the most part, their health and quality of life remains unchanged. The most notable change expressed by most living kidney donors comes in the form of the perpetual joy they feel for achieving such an extraordinary triumph.
Living kidney donors aren’t typically required to take new medications following the surgery, other than a pain medication or a stool softener for a short period of time. Kidney donors do not need to follow a special diet after they are discharged from the hospital. Likewise, they are not required to avoid alcohol, except for the period of time they would be taking pain medication. The guideline for alcohol consumption after kidney donation is fairly standard. Living kidney donors should be simply be responsible and consume alcohol in moderation.
- What emotions will the donor feel before or after surgery?
Like any excursion someone has never taken before, there can be a sense of excitement and anxiety about the journey ahead. Typically, the more one understands going into the process, the less anxiety they’ll experience. Post-surgery, most donors report a feeling of honor and joy from their heroic achievement. Remarkably, their sense of joy has reduced post-surgical pain and associated inconveniences.
- How successful are living kidney donor transplants?
Hospitals with established transplant programs show very good transplant success rates. Most transplant centers* exceed a 95% success rate one year after transplantation. The best success rates are seen in transplants from living kidney donors. (*Transplant programs are required to keep track of their success rates. Be sure to ask the center to share their success rates).
- Does the age of the donor matter?
Generally, there the ideal age range is 18-65 years old. Of course, the donor will need to prove (during their evaluation) that he or she is healthy enough to donate a kidney safely. While there have been donors who have donated a kidney after the age of 65; younger donors are preferred. Family members are also preferred, as they offer a better match. FAQ: Understanding Living Kidney Donation.
- What happens if the donor’s kidney isn’t a blood type match?
When the living kidney donor is not a match for their intended recipient (because they are incompatible in blood type or have antibodies to the recipient) they can still donate—just not directly. This is accomplished through a Paired Exchange Program.
In Paired Exchange, a computer algorithm is used to find a better match for incompatible groupings. In this model, the living kidney donor’s kidney is swapped with another person’s incompatible living kidney donor. The picture below illustrates this concept. In this scenario, a mother hoped to donate to a daughter and a brother hoped to donate to a sister. Both were unable to donate directly because it was determined that their kidneys would unlikely function well for their intended recipients. After they were told about the Paired Exchange Program, they agreed to be matched up with other incompatible pairs. In the example below, the mother donated to the brother’s sister, and the brother donated to the mother’s daughter. Though this example shows two incompatible pairs, it is not uncommon to see a larger grouping of individuals in a chained sequence of domino-like events.
- What happens if a donor changes their mind?
Interested donors can change their mind at any time about donating. Changes of this nature are kept confidential. The only information shared will be communicated as follows: “The donor was not an ideal candidate.”
- Will donating a kidney prevent the donor from getting pregnant or affect their sex life?
Donating a kidney has not shown to reduce the fertility of men or women. Because the body requires time to recover from the surgery of donating a kidney, it is recommended that women wait 3-6 months after donation to get pregnant. In the meantime, a donor can engage in sexual activities after their incisions have healed and they feel comfortable enough to do so.
- Does a kidney donor get anything for donating?
Legally, there can be no payment for kidney donation. Though, we are told that there is high value gained in the perpetual joy that comes with saving someone’s life. Some donors explain this as their highest “life achievement.” Others have called it their own “Mount Everest.” Living kidney donation is
a very personal experience. Not everyone can be a living kidney donor. It takes a very special person to connect to this humanitarian call. It also takes a very healthy person to even qualify.
- What’s the first step for someone to see if they’d qualify?
The first step is to call the kidney patient’s designated transplant center to schedule a telephone screening. During the call individuals can ask questions and get more details about the tests involved, the surgical procedure and recovery. Even if the person calling is not completely sure they want to proceed, this call can provide insight to help them decide if living kidney donation is right for them. All donor coordinator conversations are handled in strict confidence* to ensure callers can ask questions without pressure or concern. *The recipient will never know someone called in or their status, unless they tell them directly.
You Can Also Offer To Be a Back-Up
If someone has been told they are not needed (at this time), but they’re still interested in donating, they can offer to be a “backup.” This is important, should someone unexpectedly change their mind or be disqualified. (Often times, it takes several potential donors to be tested before a qualified match is found). If individuals are told they aren’t needed following the surgery, there is another way to proceed. They can also contact a hospital that performs kidney transplants in their area and tell them they’d like to be help one of their patients in need. An altruistic offer like this can often kick-off a Paired Exchange Chain. In these types of grouped events, one living kidney donor can offer extended life to a number of people in need. They do this by providing the missing link (their kidney) to be the final piece of the puzzle that completes the chain.
Key Benefits to Receiving a Transplant from a Living Donor:
- Ends the Wait
A kidney from a living donor “Ends the 3-9 Year Wait” for someone in need of a kidney transplant. The surgery can also be scheduled at the donor’s convenience when the kidney patient needs it most—and before their health declines, so they are not at risk for losing transplant eligibility.
- Offers a Better Match
Living kidney donors are thoroughly tested to ensure the best match for their recipients. Donor testing also minimizes potential risks for both the living kidney donor and the recipient.
- Offers Better Function
Kidneys from living donors are known to function immediately after transplant. They can also last twice as long as a kidney from a deceased donor. This could potentially equate into an additional 10-12 + years of function.
- Presents an Opportunity to Bypass Dialysis
Most kidney patients need to be on dialysis (to stay alive) while they wait for a deceased donor’s kidney. Hence, living kidney donors can help those in need receive a transplant before the need for dialysis. This is called a preemptive transplant. This process allows end-stage kidney disease patients to bypass* the need for dialysis altogether. *Note: Living kidney donors must be tested and approved for the surgery before the recipient’s function drops to a level of requiring dialysis.
For more information on how to become a Donor Magnet Pro, visit www.FindingKidneyDonors.com





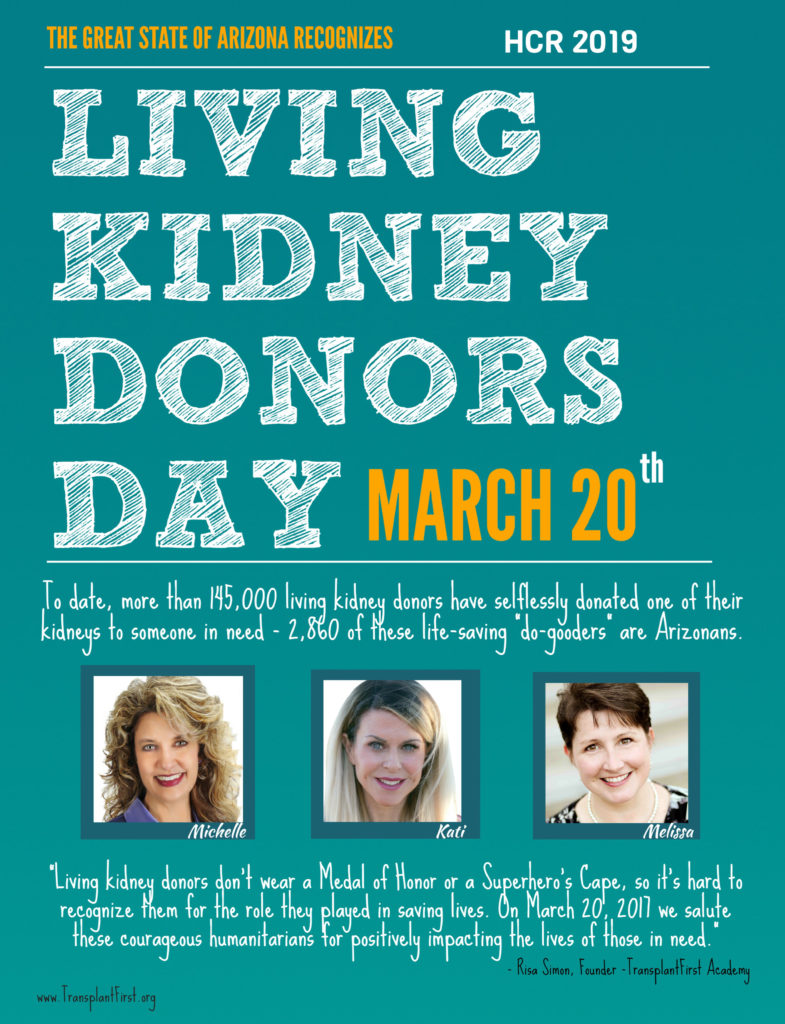
 TransplantFirst Academy is raising community awareness in living kidney donation.
TransplantFirst Academy is raising community awareness in living kidney donation. 

 Many chronic kidney disease (CKD) patients are floating in a sea of uncertainty due to inadequate patient education and various knowledge barriers. Consequently, the patient’s understanding of various treatment options—and how the timing of engagement can impact each outcome, is often lost in the shuffle.
Many chronic kidney disease (CKD) patients are floating in a sea of uncertainty due to inadequate patient education and various knowledge barriers. Consequently, the patient’s understanding of various treatment options—and how the timing of engagement can impact each outcome, is often lost in the shuffle.