
Did you know 31 million people in the US have kidney disease? Do you happen to know one of them? Wish you could help? You’re in luck—here’s 5 ways you can!
1. Keep Hydrated!
Hydration keeps kidneys strong and helps prevent kidney stones. Ensure your friends and family members with kidney disease are staying hydrated—and don’t forget to stay hydrated, as well. If they see you with a bottle, they’ll be more likely to grab one too!
2. Avoid Pain Relievers
Find ways to help someone with kidney disease relieve pain without the use of pain relieving products that are hard on your kidneys, like ibuprofen (Advil, Motrin and Nurofen), aspirin and acetaminophen. Look for neutral ways to manage pain with doctor recommended stretching, meditation and Epsom salt baths.
3. Improve Habits
Eating less protein and more vegetable along with doctor-recommended exercise are great ways to care for your body and kidneys! If they’re cigarette smokers, encourage them to put those cigarettes down!
Smoking slows the blood flow to the kidneys and can make kidney disease worse.
4. Empower Engagement
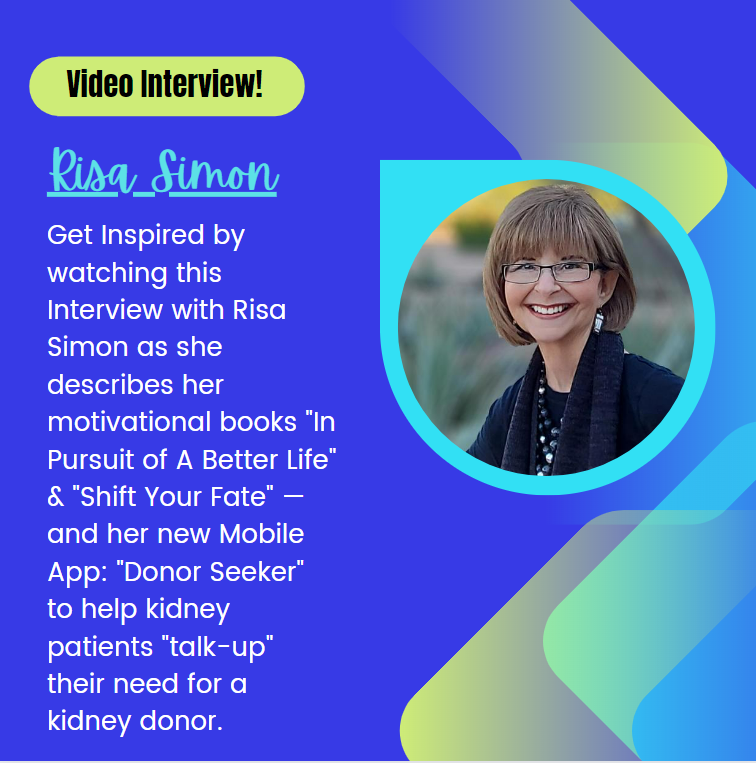
Encourage kidney disease patients to learn as much as they can about slowing the progression of their disease. Information is power. Get them engaged with their doctors by helping them prepare a list of questions before they arrive to their appointments and don’t let them leave the office until their questions have been answered satisfactorily. Are care providers teaching them how to secure their best possible outcome? Empower kidney disease patients to use their voice and become their own best advocate. Learn more here: www.shiftyourfate.com
5. Improve Outcomes
Most kidney patients don’t realize they can avoid dialysis (or end their need for dialysis) by receiving a transplant from a living kidney donor. Currently, there are 100,000 people waiting for a kidney from a deceased organ donor, with an average wait of 5 years. Living kidney donors can end the wait.
This year, less than 18,000 people of the 100,000 waiting will receive a kidney transplant. Considering these statistics, your help is needed to increase awareness and interest in living kidney donation. Get involved today.
Learn more about living kidney donation here:
Learn how to find a living kidney donor here: www.findingkidneydonors.com.
Want to learn more?
Check out these powerful books on Amazon:
Shift Your Fate: Life-Changing Wisdom for Proactive Kidney Patients
Book page: www.shiftyourfate.com
In Pursuit of A Better Life: The Ultimate Guide For Finding Living Kidney Donors Book Page: www.findingkidneydonors.com
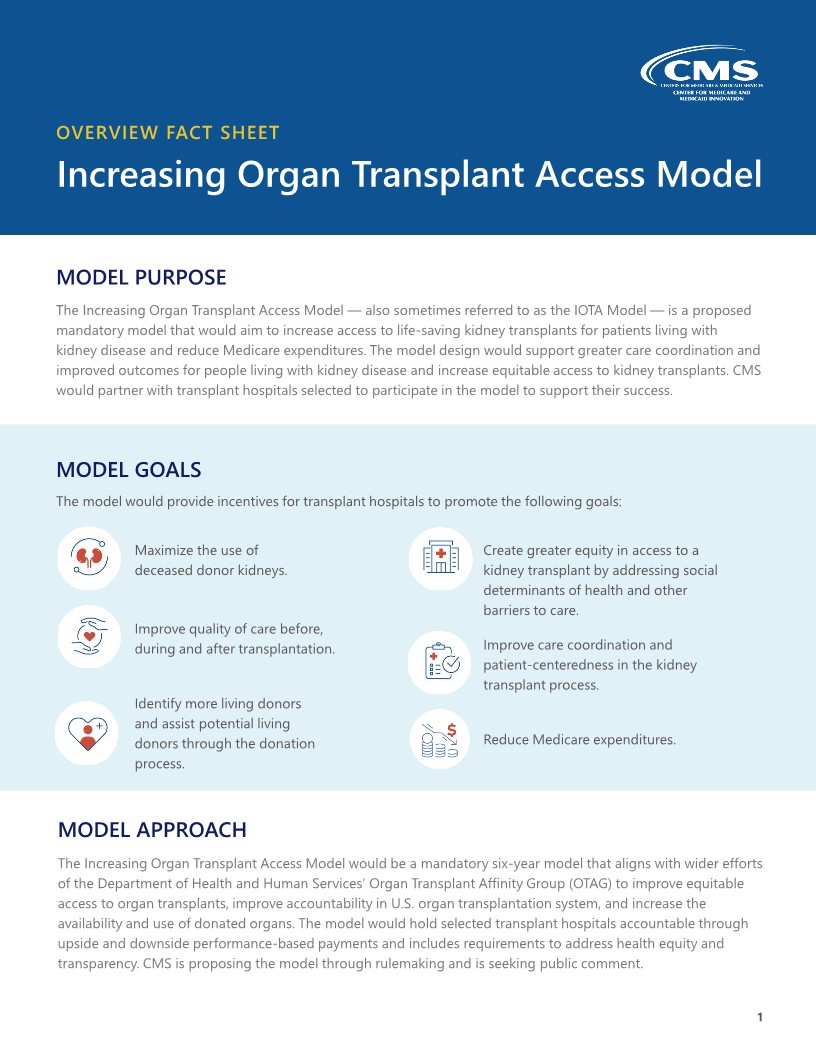




 TransplantFirst Academy is raising community awareness in living kidney donation.
TransplantFirst Academy is raising community awareness in living kidney donation.